The Center for Research and Innovation in Systems Safety (CRISS) conducts basic and applied research in healthcare informatics, patient safety and clinical quality, and designs and evaluates informatics user interfaces, care processes and medical technology across VUMC and nationally.

Directed by Matthew B. Weinger, M.D., CRISS is highly interdisciplinary and collaborative with projects spanning numerous clinical domains (from the Medical Home to the operating room) and disciplines (medicine, nursing, and pharmacy).
Using a wide range of human factors and systems engineering, cognitive psychology, biomedical informatics, and implementation science techniques, CRISS studies performance during patient care and in realistic simulations to better understand how and why care deviates from optimal. Interventions are then designed and evaluated to improve safety and care quality.
CRISS is an institution-wide resource for human factors and systems design and improvement in healthcare. We are actively involved in improving the user interfaces of Vanderbilt’s Epic-based eStar EHR and custom clinical information systems, evaluating and redesigning processes and tools to enhance patient safety and quality care, and furnishing graphic design services for research and clinical endeavors.
FOCUS
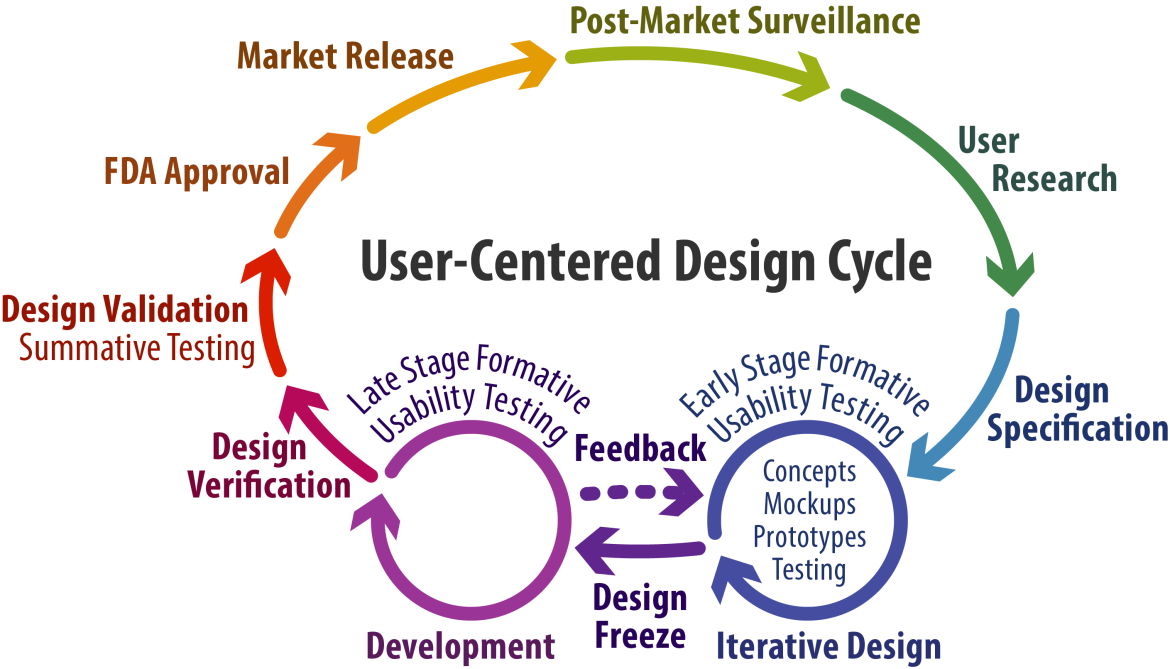
CRISS investigators are particularly interested in designing and evaluating medical technologies (i.e., devices and information systems) with an emphasis on the effects of the introduction of new technologies on clinical care and the use of electronically generated clinical data to identify evolving events and support decision-making. CRISS provides FDA- and ONC-compliant user-centered design (UCD) services, including usability testing, for external customers. We also conduct studies to understand the causes of unexpected clinical events and how such events might be prevented.
At the conceptual level, CRISS scientists are interested in the nature of expertise, system complexity, clinician-clinician communication, novel methods of information presentation, the workload and stress of individual clinicians and of teams, situational awareness, and various other intrinsic and extrinsic variables that affect performance during routine and non-routine clinical care.
CRISS investigators are also interested in team communication, coordination, culture and effectiveness, human-technology interactions, adaptive problem solving, as well as individual and group performance-shaping factors, to generate practical benefits in terms of improved clinical care processes and outcomes.
We are fundamentally interested in how best to positively affect individual (i.e., clinicians and patients) and organizational behaviors to advance human health.
Advancing Medical Simulation
CRISS is the Coordinating Center and host for the Simulation Assessment Research Group (SARG). SARG is a U.S. national multidisciplinary consortium of researchers and educators interested in the use of medical simulation to study clinical performance, expertise, decision making, and education, primarily in the context of the management of critical or crisis events. To date, SARG has focused on anesthesiology although the findings are applicable to other acute care specialties (e.g., emergency medicine, critical care, surgery) and are likely generalizable to non-medical domains (e.g., aviation, military, firefighting).
International Collaboration
In 2022, CRISS signed a formal collaboration agreement with the Hospital virtual Valdecilla (HvV) in Santander, Cantabria, Spain. HvV is a simulation, patient safety, and human factors research and education center affiliated with the government of Cantabria, the Marqués de Valdecilla University Hospital, and the University of Cantabria.

The goals of this collaboration include:
- Promote the knowledge and skill development of both institutions' personnel in human factors, patient safety, and systems science with an initial focus on Human Factors approaches to care process improvement, adverse event detection and analysis, and advanced approaches for clinical training.
- Improve Human Factors tools and methods to conduct research at HvV on process improvement and patient safety.
- Develop strategies for research projects and programs that are of joint interest.
- Host collaboration visits by VUMC faculty at HvV (Dr. Banerjee visited HvV in February 2022) and by HvV faculty at VUMC in 2023-24 to strengthen the ties between our two organizations.
History
Because of increasing scope and impact outside the operating room and across multiple healthcare domains, the Center for Perioperative Research in Quality (CPRQ), founded in 2005, was renamed in October 2010 to be the Center for Research and Innovation in Systems Safety. CRISS remains located within the Department of Anesthesiology, and is an integral part of Vanderbilt’s Institute for Medicine and Public Health (IMPH), founded by Dr. Robert Dittus and currently directed by Dr. Russell Rothman, within the Centers for Health Services Research under Dr. Sunil Kripilani. The Center also subsumed the functions of Vanderbilt’s Center for Improving Patient Safety (CIPS).



